This is in my back yard in the OC and for a few doctors I know this just might be the big push to start a Concierge Medical Office. Newport Beach which is south of  where I live has a ton of affluent residents and the Boutique practices there do well as money for many in the area is not a problem. Monarch has been around for many years and they are at all the Hoag Hospital money raising events and is very active, so things might be changing in time.
where I live has a ton of affluent residents and the Boutique practices there do well as money for many in the area is not a problem. Monarch has been around for many years and they are at all the Hoag Hospital money raising events and is very active, so things might be changing in time.
What will be interesting though is to see if the reimbursement changes and of course that’s at the top of every MD’s mind, so I don’t see much excitement about this at all here. I know have friends that won’t be excited with the news who are patients. Back in March of this year they closed a big office in Orange County and you can read more about how that went down, employees bused to a hotel and given their papers after an instant message.
With 2300 doctors in the HMO, with recent mergers and acquisitions is this a basket full of doctors to sell an EHR too as they do sell and have sold a medical records system for years under the former name of Ingenix, now known as Optum. Sometimes you run into situations like this to where one division of a big conglomerate cuts rates with one subsidiary and then the other rushes in to sell software.
Also the company recently bought another huge HMO group in Long Beach and I would say the two are perhaps close in size but bottom line is both are huge
We never did get our government REC center started in the OC either and I just kind of wonder where the money went on that too, and again with the post above with selling medical records, does this give anyone an unfair advantage for sales? It does make you wonder and again why the REC center never got off the ground and I’m just speaking out loud here but there’s no REC center to offer any help to the doctors in the OC.
I have heard from a few doctors on how the deductions of claims that get  rescinded after payment have been a hassle with United as they just take a deduction out of a check and the claim that is not being paid does not even include the patient who is being denied, a nightmare for doctors and a recent study said it costs a doctor about $83k a year to keep up with the likes of all of this. We have one first class hospital that kicked United out the door when it came to employer provided insurance and companies all over the OC were looking for another carrier when the United/Pacificare contracts were re-negotiated.
rescinded after payment have been a hassle with United as they just take a deduction out of a check and the claim that is not being paid does not even include the patient who is being denied, a nightmare for doctors and a recent study said it costs a doctor about $83k a year to keep up with the likes of all of this. We have one first class hospital that kicked United out the door when it came to employer provided insurance and companies all over the OC were looking for another carrier when the United/Pacificare contracts were re-negotiated.
I guess Hoag Hospital though is happy to have the affluent residents to help make up for the other side of things as who knows how new contracts will end up shaking out when they come up for renewal. When it comes to patents too with Health IT, United is right up there too so things don’t come cheap in that department or some subsidiaries either.
And here’s a few more back posts on their subsidiaries…think they are only insurance, well they are very heavily invested in Health IT these days as well and the acquisitions have been steady for them over the last 3 years or so.
“OptumHealth offers three types of HSAs, as well as tax-advantaged health care  savings and spending accounts, debit-card services, benefits administration services, and payment products. About three-quarters of the bank’s 1.6 million accounts are employer-generated, while the other quarter are individual accounts.”
savings and spending accounts, debit-card services, benefits administration services, and payment products. About three-quarters of the bank’s 1.6 million accounts are employer-generated, while the other quarter are individual accounts.”
There’s also the Chinese investment the company bought early in 2010.
These are just a few examples of some of the subsidiaries of the company and why even sometimes judges find themselves in some potential conflict areas as the daisy chains of subsidiaries grow, they don’t even keep track or are cognizant that the company they have owned stock in for many years, due to quickly adapting business algorithms used today, is not the same. The former Ingenix division (now Optum) makes money with pretty much just selling data and creating software algorithms.
Back a year or so ago the AMA fought and won a lawsuit against the Ingenix division for short paying doctors and patients for almost 15 years and it was Andrew Cuomo of New York who got the ball rolling there. In some parts of the country through wellness subsidiaries pharmacists even get to earn pay for performance money from signing people up in wellness programs, and what that amount is we don’t know but the retail drug chain, Walgreens says their data selling business is worth just under $800 Million.
Last but not least, let’s not forget the CEO is the highest paid in the US for public companies, and they are still making record profits. I just try to break down the business areas for awareness so consumers and others understand a bit more about the big corporate world of subsidiaries today that normally may not be thought about, seen or recognized. BD
UnitedHealth Group Inc. will acquire the operations of a major southern California physician group, in the latest example of how lines are blurring between insurance companies and health-care providers.
The purchase of the management arm of Monarch HealthCare, an Irvine, Calif., association that includes approximately 2,300 physicians in a range of specialties, establishes United's Optum health-services unit as a formidable presence in the region. Optum had previously taken over the management arms of two smaller southern California groups, AppleCare Medical Group and Memorial HealthCare Independent Practice Association.
Monarch said in a statement that it "has agreed to enter a strategic relationship with Optum to support our physicians in providing high-quality, cost-effective patient care in Orange County, California."
United has said in the past that providers acquired by Optum will not work exclusively with United's health plan, and will continue to contract with an array of insurers. But in one sign of the potential complications that might ensue, Monarch is currently in an arrangement with United competitor WellPoint Inc. to create a cooperative "accountable-care organization" aimed at bringing down health-care costs and improving quality.
 million for their portion of gaining market share.
million for their portion of gaining market share. 


 part of the deal here as that’s the way it works out there today with everyone wanting data. Another division of United sells prescription data for underwriting and other purposes.
part of the deal here as that’s the way it works out there today with everyone wanting data. Another division of United sells prescription data for underwriting and other purposes. 
 State Insurance Exchange solutions. Microsoft’s HIX solutions eliminate the need for states to evaluate numerous point solutions from various firms to find one that works well with government policies or existing IT infrastructures.
State Insurance Exchange solutions. Microsoft’s HIX solutions eliminate the need for states to evaluate numerous point solutions from various firms to find one that works well with government policies or existing IT infrastructures.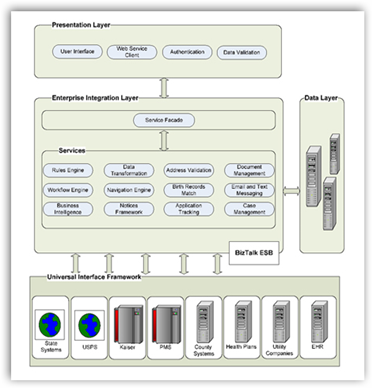



 where I live has a ton of affluent residents and the Boutique practices there do well as money for many in the area is not a problem. Monarch has been around for many years and they are at all the Hoag Hospital money raising events and is very active, so things might be changing in time.
where I live has a ton of affluent residents and the Boutique practices there do well as money for many in the area is not a problem. Monarch has been around for many years and they are at all the Hoag Hospital money raising events and is very active, so things might be changing in time.  Compensation Contracts Using One Subsidiary Then Market Same MDs With Another Subsidiary in Health IT
Compensation Contracts Using One Subsidiary Then Market Same MDs With Another Subsidiary in Health IT rescinded after payment have been a hassle with United as they just take a deduction out of a check and the claim that is not being paid does not even include the patient who is being denied, a nightmare for doctors and a recent study said it costs a doctor about $83k a year to keep up with the likes of all of this. We have one first class hospital that kicked United out the door when it came to employer provided insurance and companies all over the OC were looking for another carrier when the United/Pacificare contracts were re-negotiated.
rescinded after payment have been a hassle with United as they just take a deduction out of a check and the claim that is not being paid does not even include the patient who is being denied, a nightmare for doctors and a recent study said it costs a doctor about $83k a year to keep up with the likes of all of this. We have one first class hospital that kicked United out the door when it came to employer provided insurance and companies all over the OC were looking for another carrier when the United/Pacificare contracts were re-negotiated. savings and spending accounts, debit-card services, benefits administration services, and payment products. About three-quarters of the bank’s 1.6 million accounts are employer-generated, while the other quarter are individual accounts.”
savings and spending accounts, debit-card services, benefits administration services, and payment products. About three-quarters of the bank’s 1.6 million accounts are employer-generated, while the other quarter are individual accounts.”


 hospitals as sometimes the reimbursement efforts left them out of pocket to cover the cost of the drugs up front and then fighting a claim later to get paid. In the survey,some doctors also mentioned that the cost for such drugs should not go over $60,000 while others said that $10,000 should be the cap.
hospitals as sometimes the reimbursement efforts left them out of pocket to cover the cost of the drugs up front and then fighting a claim later to get paid. In the survey,some doctors also mentioned that the cost for such drugs should not go over $60,000 while others said that $10,000 should be the cap. 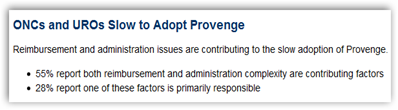
 additional surveys to follow but the question of reimbursement is big and rightly so, how can we afford the drugs as even with insurance there’s still some big potential cost involved here. One more tidbit here relative to Provenge which was in the news of late as the FDA just approved another facility, however it looks like they will be laying people off. If you have followed the development of the drug over the last 3 years with all the news, it has been a rocky, bumpy and political ride. BD
additional surveys to follow but the question of reimbursement is big and rightly so, how can we afford the drugs as even with insurance there’s still some big potential cost involved here. One more tidbit here relative to Provenge which was in the news of late as the FDA just approved another facility, however it looks like they will be laying people off. If you have followed the development of the drug over the last 3 years with all the news, it has been a rocky, bumpy and political ride. BD 




 town hall meeting as in my area in the OC which is a GOP rep we get robocalls…”hi..I’m….and so you glad you could be on the line to talk with me tonight”…disgusting and pretty useless and they talk more about the tomato plants on the office patio than anything else.
town hall meeting as in my area in the OC which is a GOP rep we get robocalls…”hi..I’m….and so you glad you could be on the line to talk with me tonight”…disgusting and pretty useless and they talk more about the tomato plants on the office patio than anything else. 


 timeline and data decisions, who don’t do any of this themselves!! Get a clue soon, please! Non participant executives who don’t understand Health IT and data flows are killing us as they don’t get it and have absolutely “no hands on” experience to help them in this area.
timeline and data decisions, who don’t do any of this themselves!! Get a clue soon, please! Non participant executives who don’t understand Health IT and data flows are killing us as they don’t get it and have absolutely “no hands on” experience to help them in this area.  County, California either, and I guess they got the money but zero has been done and their information page is still part of the over all Cal-Optima Medicaid insurance site as that’s who received the contract.
County, California either, and I guess they got the money but zero has been done and their information page is still part of the over all Cal-Optima Medicaid insurance site as that’s who received the contract.  his toe, so I said “Get on Skype put your toe up there”. You can read more at the link below, but gee, why not? Both the doctor and friend were happy with the suggestion and Skype is so widely known already too. They had a great foot conference out of this:)
his toe, so I said “Get on Skype put your toe up there”. You can read more at the link below, but gee, why not? Both the doctor and friend were happy with the suggestion and Skype is so widely known already too. They had a great foot conference out of this:) the meantime it’s Redneck healthcare, but it works! Back when I wrote this a few months ago, Microsoft here in the US said they were also looking at incorporating Skype where they could but it may be a while before we hear anything but in the meantime, the NHS is hot after the trail of using Skype. This is a big deal as you don’t have to sell the consumers and doctors on “value” either, it’s automatically recognized, unlike so much other software and programs that float around out there today too. We are so over done with technologies that offer mobile apps that only do “one thing”, a huge glut and the stuff keeps coming. I rant about it all the time and most of the developers that create consumer software don’t even think about using themselves to make matters worse. We have ton of innovation in the US, but a big lack of collaboration.
the meantime it’s Redneck healthcare, but it works! Back when I wrote this a few months ago, Microsoft here in the US said they were also looking at incorporating Skype where they could but it may be a while before we hear anything but in the meantime, the NHS is hot after the trail of using Skype. This is a big deal as you don’t have to sell the consumers and doctors on “value” either, it’s automatically recognized, unlike so much other software and programs that float around out there today too. We are so over done with technologies that offer mobile apps that only do “one thing”, a huge glut and the stuff keeps coming. I rant about it all the time and most of the developers that create consumer software don’t even think about using themselves to make matters worse. We have ton of innovation in the US, but a big lack of collaboration.